Abstract
Introduction: Acute(aGVHD) and chronic graft-versus-host disease (cGVHD) cause significant morbidity and mortality in patients post hematopoietic cell transplantation (HCT). The use of T-replete HLA-haploidentical transplantation (HIDT) with post-transplant cyclophosphamide has become a common donor source for patients lacking a suitably matched donor. In spite of the increase in HIDT, there is paucity of data describing aGVHD and cGVHD outcomes and potential risk factors for developing graft-versus-host disease after HIDT.
Methods: The outcomes and the characteristics of 203 patients undergoing first allogeneic transplantation using HIDT with post-transplant cyclophosphamide between 2005 and 2016 were retrospectively assessed to identify the incidence and risk factors for aGVHD and cGVHD. Variables included in the analysis included patient related (age, sex, race, karnofsky, HCT-CI), disease related (diagnosis, disease type, disease risk index DRI, CIBMTR risk status) and transplant related (graft source as marrow vs peripheral blood, donor age, donor/recipient relationship, donor/recipient gender match, donor/recipient CMV match, conditioning intensity, high dose TBI in conditioning intensity, CD34 cell dose, CD3 cell dose and year of transplant). Univariate analysis with Gray's test and log-rank was carried for cumulative incidence and survival respectively. The proportional hazard cox model was used with backward elimination to select significant covariates. Multivariate analyses for developing GVHD, overall survival (OS), disease free survival (DFS), and relapse were conducted.
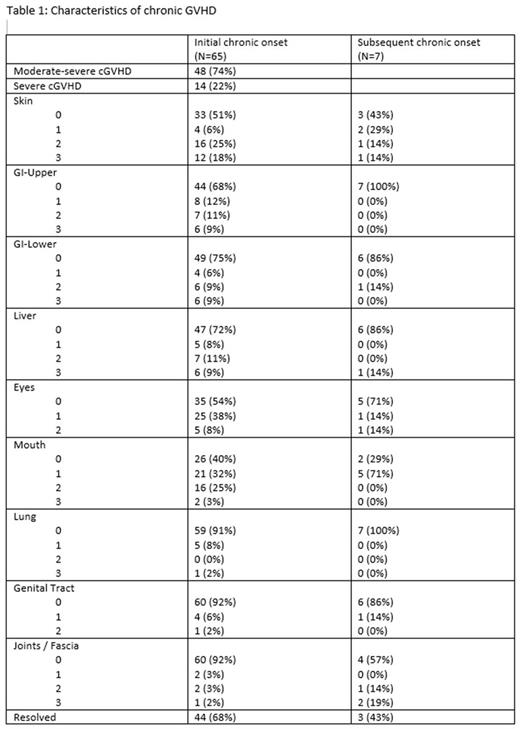
Results: The median age was 51 years (range 19, 75) with a median follow up for survivors of 37 months. Seventy patients (34%) received bone marrow as graft source and 43% had Myeloablative conditioning. All patients received GVHD prophylaxis consisting of post-transplant cyclophosphamide on Days +3 and +4, MMF till day +35 and tacrolimus till day +180. The cumulative incidence for aGVHD grade II-IV and grade III-IV were 45% and 12% respectively. The common organs involved in aGVHD were skin (76% of cases, 39% stage 3 /4), gut (58% of cases, stage 3 /4 11%) and liver (7% of cases, stage 3 /4 of 1%). Subsequent aGVHD flare developed in 6 patients (5 with gut GVHD and 1 skin GVHD). The cumulative incidences of all grade cGVHD and moderate-severe cGVHD were 32% and 24% respectively (table 1). Conditioning intensity was the only risk factor associated with developing grade 2-4 aGVHD (p=0.04). Patients that received myeloablative regimens as compared to those who received a reduced intensity or non-myeloablative regimen had statistically higher rates of grade 2-4 aGVHD (hazard ratio [HR] of 1.52 (95% CI, 1.01-2.29, p=0.04). Risk factors for cGVHD showed that race and hematopoietic cell transplantation-comorbidity index (HCT-CI) had a statistically significant bearing on the likelihood of developing all-grade cGVHD (p=0.004 and 0.01 respectively). Graft source (marrow vs Peripheral blood) was a significant risk factor for developing moderate-severe cGVHD (p=0.03). Multivariate analysis on OS, DFS and relapse showed that Patients aged 55 or older (HR of 1.91, 95% CI 1.22-2.99, p =.005) and High/very high DRI risk (HR 2.06, CI 1.05-4.00, p=0.03) had worse overall survival rates. Older age, not developing chronic GVHD and receiving a transplant between 2005 and 2010 were all associated with a worse DFS (P<0.01 for all). High/very high DRI, male gender and not developing cGVHD were all significant factors for a higher relapse rate.
Conclusions: This single center analysis of GVHD incidence and risk factors after HIDT using post-transplant cyclophosphamide showed that conditioning intensity, graft source and HCT-CI to be factors affecting incidence of GVHD. Higher disease risk and older patient age were associated with worse overall survival.
Solh: Amgen: Speakers Bureau; ADC Therapeutics: Research Funding; Celgene: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.